'Cold' Carriers to up travel time for transplant hearts

You cannot blame transplant surgeons for having high BP. After all, speeding in an ambulance across the city, removing a beating heart (or liver or lung) from a brain-dead patient, putting it in a box of saline and rushing back before the organ gets infected or stops beating... and then operating for 6-12 hours, cannot be good for the nerves.
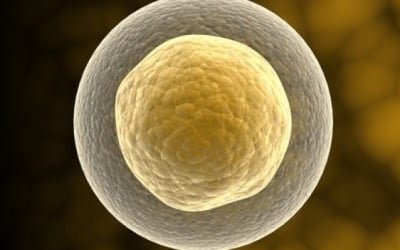
The heart transplant team at Global Health City may be able to breathe a little easier soon, when they procure new organ transportation cases that are equipped with cold perfusion technology. “Right now, the organs are carried in sterilized boxes with ice and saline, which keep the organ usable for up to four hours. But the battle against time is a constant worry,” said Dr R Ravi Kumar, senior interventional cardiologist at the hospital.
Despite its having the best organ transplant programme in the country, at least a 100 harvested organs go to waste every year, rued cardiologist Dr Nandkishore Kapadia at the inauguration of Global’s Heart Failure Clinic on Wednesday. Most of it is because the organ gets infected before it reaches the recipient.
In contrast, the cold perfusion boxes will keep feeding the heart cold nutrients that circulate inside the blood-pumping organ, allowing it to stay alive and fresh for longer. “Studies have indicated that these cases will be able to keep harvested cadaver hearts alive for up to nine hours,” he added about the boxes which have been procured at a cost of `60 lakh. (more than $100,000 U.S.)
While the additional time will make it easier for ambulance drivers who battle the city’s traffic every day, what it really does is open up the possibility of procuring organs from further south. “At the moment, we struggle to procure organs from Tiruchy, which is about three hours away through our ‘green corridor’. With the advantage of these boxes, we may be able to receive organs from places like Coimbatore soon,” said Dr Ravi.
Global’s Heart Failure Clinic brings together the whole gamut of heart services from elective surgeries to emergencies in one department and is among the few of its kind in the country.
Source: By
April is Organ Donor Month
“You Have the Power to Donate Life – Sign-up today! Tell Your Loved Ones of Your Decision”
Donor Registration Links in your home country